By ANEEKA SIMONIS
HEALTH laws are taking police off the streets to look after dangerous volatile psychotic patients, many high on ice, for up to eight hours a time.
An emergency services worker, who asked not to be identified, said skyrocketing hospital admission rates for mentally unwell patients was “out-of-control”, particularly in the Cardinia Shire and Greater Dandenong region.
They said that hospital staff and police are at odds with each other over the issue, with many police officers growing frustrated with laws requiring them to mind drugged or volatile patients for hours at a time as they wait to be seen by emergency health staff.
In some cases, police are being accused of dumping patients at hospitals so they can carry on with their other duties.
A hospital diversion system co-ordinated by police and psychiatric staff was introduced to relieve pressure on the region’s public health system, but it appears the program is also struggling to keep up.
In the past 18 months, the Police, Ambulance and Critical Early Response (PACER) unit servicing the southern metropolitan region, including the Cardinia, Casey and Greater Dandenong region, has been called to intervene in more than double the cases seen since its inception.
Police have made unsuccessful funding requests to expand the single vehicle unit’s current hours of 3pm and 11pm daily.
Under Section 351 of the Mental Health Act, police are required to stay with psychosis patients until they are under the care of emergency medical staff.
Police already struggling to keep up with demands on their under-resourced unit are being increasingly called out to transfer and ‘babysit’ these patients as they wait for medical help in the southern metropolitan region.
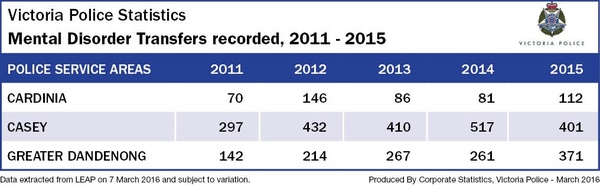
Last year, police recorded a 38 per cent increase in mental disorder hospital transfers from the Cardinia shire region – 112 transfers in 2015 compared with 81 in 2014.
The increase was even greater in the Dandenong region, with police recording 371 mental health transfers in 2015 compared with 261 in the previous 12-month period – up 42 per cent.
Victoria Police does not keep a record of the number of drug-affected transfers assisted by police although crime statistics show drug use and possession offences were up more than a quarter in Cardinia Shire last year.
It was a greater than average increase recorded state-wide.
The trend was no better across the entire southern metro division.
Greater Dandenong recorded a 23 per cent increase in overall drug offences in 2015 and a similar rise was recorded in Casey.
 Police Association secretary Ron Iddles said officers were spending between four and eight hours in hospital emergency departments minding mental health patients.
Police Association secretary Ron Iddles said officers were spending between four and eight hours in hospital emergency departments minding mental health patients.
It pulls already “critically low levels” of police members off the streets, according to Mr Iddles who is calling for a change to hospital admission practices.
The situation has been compounded by Victoria Police’s two-up policy which requires officers to work in pairs.
He said it was crucial that hospital systems were reworked to free up police.
“Hospitals need to be provided with adequate resources and security personnel to enable this to happen,” he said.
“Police need to be released from hospital waiting rooms quickly so that they can respond to urgent calls for assistance,” he said.
PACER has attended more than 4000 incidents in Cardinia Shire, Casey and Dandenong in the past five years.
The unit has helped divert between 70-80 per cent of mental health patients from being admitted to hospital by providing ‘on the spot’ crisis intervention care to reduce the demand on hospitals including Casey Hospital and Dandenong Hospital.
Victoria Police has responded to concerns about the overworked unit.
Superintendent Paul Hollowood confirmed the program was under review.
“We are in the process of investigating and reviewing a variety of integrated services and responses in our region, including PACER,” he said.
“While it is too soon to pre-empt the outcomes of that piece of work, as it stands the PACER unit is continually monitored and adjusted to ensure it is meeting the needs of the community.”
A spokesperson for the Department of Health and Human Services said PACER units rolled out across the state’s most high-demand mental health areas had helped reduce dependence on hospital emergency departments.
However, the department provided no answer to funding calls for the expanded south-east PACER unit.
A recent Gazette investigation found that Casey Hospital’s facilities and security system are forcing aggressive, sometime drug-addled patients, to sit side by side during their wait for medical care.
An off-the-record emergency health worker blamed the hospital’s poor facilities, including a lack of isolated rooms, and security management system, for the issue.
The hospital’s security personnel are employed to protect the building rather than intervene during violent crises unlike security teams at Dandenong Hospital which are there to protect patients.
“It’s unsafe for the general public and it’s unsafe for mental health patients,” the source said.
The lack of in-house security means police are called in to contain violent situations, though their powers are compromised.
“You can’t let off a can of OC (capsicum) spray on someone when there is someone else suffering from a heart attack next to them,” the emergency health worker said.
A Monash Health spokesperson said patients were assessed on arrival.
“On arrival at Casey Hospital Emergency Department, patients are assessed so that they can receive the most appropriate care in the most suitable area of the department,” the spokesperson said.
“The safety of our patients and our staff is a priority.”
Ambulance Victoria has recently revealed that some homes in the south-east region were being blacklisted after violence against staff.
They include 34 in Dandenong, 22 in Cranbourne, 15 in Noble Park, 11 in Hampton Park, 10 in Narre Warren and nine in Pakenham.
Paramedics called to these addresses will not treat patients until police are on scene.
Anyone in need of help is urged to contact Lifeline on 13 11 14 or beyondblue on 1300 224 636.